Receiving unexpected news about your health can be incredibly daunting, often leaving you with a swirl of questions and anxiety. If you’ve been told about or are investigating Endometrial Hyperplasia, you’re likely navigating this very real stress. Rest assured, understanding the journey ahead is the first, most powerful step towards regaining control.
So, what exactly is Endometrial Hyperplasia? In simple terms, it’s a condition where the lining of your Uterus – the Endometrium – becomes unusually thick. This often occurs due to an imbalance, specifically an excess of Estrogen without sufficient progesterone to keep it in check. The most common red flag that sends many women to their Gynecologist? Persistent or unusual Abnormal Uterine Bleeding.
But how do doctors figure out what’s really going on? This guide is designed to empower you, walking you through the entire diagnostic process. We’ll break down the 5 crucial steps, from your initial consultation to deciphering the final Pathology Report, ensuring you’re informed and prepared every step of the way.
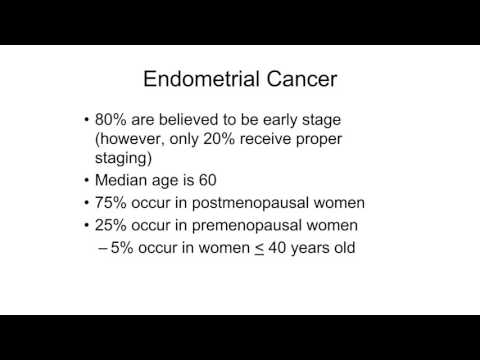
Image taken from the YouTube channel Huntsville Hospital , from the video titled Endometrial Hyperplasia & Carcinoma .
Embarking on any health journey can feel overwhelming, especially when faced with unexpected concerns that bring new terms and uncertainties into your life.
When the Unforeseen Arrives: Beginning Your Journey with Endometrial Hyperplasia
Receiving news about an unexpected health condition can be a challenging moment, often filled with a mix of emotions—confusion, worry, and perhaps a sense of being overwhelmed. It’s completely normal to feel this way, especially when terms like ‘Endometrial Hyperplasia’ are new and unfamiliar. Our aim here is to offer you a compassionate guide, demystifying the diagnostic process and empowering you with the knowledge to navigate this path with greater clarity and confidence.
Decoding Endometrial Hyperplasia: What It Means for Your Uterus
At its heart, Endometrial Hyperplasia is a condition that affects the Uterus, specifically its inner lining, known as the Endometrium. Think of the endometrium as a soft, nutrient-rich cushion that builds up each month in preparation for a potential pregnancy. If pregnancy doesn’t occur, this lining is shed during menstruation.
In cases of Endometrial Hyperplasia, this delicate balance is disrupted. The condition occurs when the Endometrium becomes too thick. This often happens due to an excess of Estrogen in the body, without enough Progesterone to balance its effects. Estrogen is responsible for building up the endometrial lining, while progesterone helps to stabilize it and prepare it for shedding. When estrogen dominates without sufficient progesterone, the endometrial cells can grow excessively, leading to the thickening that defines hyperplasia. It’s an overgrowth of these cells, which, in some forms, can be a precursor to uterine cancer if left untreated.
The Body’s Signal: Understanding Abnormal Uterine Bleeding
For many, the first and most common sign that prompts a visit to a Gynecologist is Abnormal Uterine Bleeding. This isn’t just a slightly heavier period; it refers to bleeding that is outside of your usual menstrual pattern. It might manifest as:
- Periods that are much heavier or longer than usual.
- Bleeding between periods.
- Spotting or bleeding after menopause (which should always be investigated promptly).
- Irregular menstrual cycles that suddenly become unpredictable.
This abnormal bleeding occurs because the overly thickened Endometrium becomes unstable and sheds irregularly, rather than in a controlled monthly cycle. Recognizing these changes in your body and seeking professional advice is a crucial first step toward understanding what’s happening and getting the care you need.
Your Path Forward: An Overview of the Diagnostic Journey
To help demystify the path ahead, we’ll outline the five key steps involved in diagnosing Endometrial Hyperplasia. Understanding this journey can help you feel more prepared and in control, knowing what to expect from your initial consultation right through to understanding your final results.
- Your Initial Consultation and Symptom Recognition: This is where you discuss your symptoms and medical history with your gynecologist.
- Further Investigations: Imaging and Clinical Assessment: Your doctor may recommend a physical exam and imaging tests, such as a pelvic ultrasound, to get a clearer picture.
- The Essential Step: Endometrial Biopsy: A small tissue sample is taken from the uterus for microscopic analysis.
- Pathology Review: Understanding the Tissue Results: A pathologist examines the biopsy to determine the specific type and severity of hyperplasia.
- Diagnosis Confirmation and Initial Discussion of Next Steps: Your doctor will explain your specific diagnosis and discuss the initial treatment considerations.
Understanding these initial steps is the first stride on your path to clarity, beginning with recognizing the signals your body sends and your crucial first meeting with your gynecologist.
Understanding your health journey begins with noticing the subtle (or not-so-subtle) changes in your body, a vital first step in diagnosing conditions like endometrial hyperplasia.
When to Listen: Recognizing Your Body’s Signals and Your First Gynecologist Consultation
The earliest and most significant indicator that something might be amiss with your uterine lining is often a change in your menstrual pattern or any unusual bleeding. Recognizing these signals and taking the courageous step to consult a healthcare professional is paramount.
Understanding Abnormal Uterine Bleeding: The Primary Signal
The most common symptom of endometrial hyperplasia is abnormal uterine bleeding (AUB). This isn’t just about a slightly different period; it encompasses a range of changes that warrant attention. Your uterus is communicating with you, and understanding these forms of AUB is crucial.
Here are the primary ways abnormal uterine bleeding might manifest:
- Heavier or Longer-than-Usual Periods: You might notice your periods lasting more days than before, requiring more frequent pad or tampon changes, or involving passing larger blood clots.
- Bleeding Between Periods (Intermenstrual Bleeding): Any spotting or bleeding that occurs outside of your regular menstrual cycle, no matter how light, should be noted.
- Any Postmenopausal Bleeding: If you have gone through menopause (defined as 12 consecutive months without a period) and experience any vaginal bleeding, it is never considered normal and always requires immediate medical evaluation.
To help you better identify these signals, here is a table outlining common symptoms:
| Symptom of Endometrial Hyperplasia | Brief Description |
|---|---|
| Heavy Menstrual Bleeding | Periods that are significantly heavier or require more frequent protection. |
| Prolonged Periods | Menstrual cycles that last longer than your usual duration. |
| Bleeding Between Periods | Any spotting or bleeding occurring when you are not expecting your period. |
| Postmenopausal Bleeding | Any vaginal bleeding experienced after you have reached menopause. |
| Pelvic Pain/Discomfort | While less common, some women might experience mild discomfort or pressure in the lower abdomen. |
Preparing for Your Important Conversation
We understand that discussing personal health concerns can feel daunting, but preparing for your initial gynecologist appointment can make it much more productive and less stressful. This appointment is your opportunity to share your observations and concerns thoroughly.
- Track Your Symptoms: Before your visit, try to keep a brief log or diary of your bleeding patterns. Note the dates of bleeding, how heavy it was, how long it lasted, and any associated pain or other symptoms. This detailed information will be incredibly helpful to your doctor.
- Prepare Your Questions: Jot down any questions or concerns you have. This ensures you remember everything you want to ask during your consultation. Common questions might include: "What could be causing this bleeding?", "What tests might be needed?", or "What should I expect next?"
The Pelvic Exam: What to Expect
During your initial consultation, your gynecologist will likely perform a pelvic exam. This is a standard and essential part of assessing your reproductive health. While it might feel a little uncomfortable, it’s generally not painful and provides crucial information.
During a pelvic exam, your doctor will:
- Visually inspect your vulva and vagina.
- Use a speculum to gently open the vaginal walls, allowing them to visualize your cervix. They might take a Pap test during this time, if due.
- Perform a bimanual exam, where they insert gloved fingers into your vagina while gently pressing on your abdomen. This allows them to feel the size, shape, and position of your uterus and ovaries, helping to detect any abnormalities.
This exam helps your doctor assess the overall health of your uterus, ovaries, and other pelvic organs, offering initial clues about any potential issues.
Your Medical History: A Crucial Piece of the Puzzle
Sharing your complete medical history is incredibly important. Your gynecologist will ask about your menstrual cycles, pregnancies, past medical conditions, and any medications you are taking. Be sure to also highlight any factors that could increase your risk of endometrial hyperplasia, especially those related to estrogen exposure.
These risk factors can include:
- Obesity
- Polycystic Ovary Syndrome (PCOS)
- Never having been pregnant
- Early menstruation or late menopause
- Certain types of hormone therapy (e.g., unopposed estrogen therapy)
- Tamoxifen use (a medication for breast cancer)
- A family history of uterine, ovarian, or colon cancer
Providing a comprehensive medical history allows your doctor to connect the dots and develop the most appropriate diagnostic plan for you.
Once your doctor has a clear understanding of your symptoms and medical history, they will consider the next steps in gaining a clearer picture of your uterine health.
After your initial discussion with your Gynecologist and a physical examination, the next logical step in understanding your symptoms is to gain a more detailed view of your reproductive organs.
Unveiling the Inner Landscape: What a Transvaginal Ultrasound Shows
When concerns arise about the health of your reproductive system, particularly regarding the uterine lining, your Gynecologist will often recommend a Transvaginal Ultrasound. This essential diagnostic tool provides a clearer, more intimate look than external methods, helping to guide your care pathway with precision and confidence.
What is a Transvaginal Ultrasound?
A Transvaginal Ultrasound is a specialized imaging test that uses sound waves to create pictures of the uterus, ovaries, and fallopian tubes. Unlike a standard abdominal ultrasound, this procedure offers a much closer view of these organs, which is crucial for detailed assessment.
- How it’s Performed: During the procedure, you’ll lie on an examination table, similar to a pelvic exam. Your Gynecologist or a trained sonographer will gently insert a small, lubricated probe (transducer) into your vagina. This probe emits high-frequency sound waves that bounce off your internal organs. These echoes are then translated into real-time images displayed on a monitor. While some may experience mild pressure, it’s generally not painful and is a quick procedure, typically lasting only 15-30 minutes.
- Why It Provides a Detailed View: The close proximity of the transvaginal probe to the pelvic organs allows for incredibly clear and detailed images. This "inside look" is superior for assessing the texture, size, and specific characteristics of the reproductive organs, including the vital lining of the uterus.
Measuring the Endometrial Stripe: A Key Indicator
One of the primary focuses of a Transvaginal Ultrasound when investigating potential issues like irregular bleeding is the measurement of the Endometrium. The Endometrium is the inner lining of the uterus that thickens and sheds during the menstrual cycle.
- The Endometrial Stripe: On an ultrasound, the Endometrium appears as a distinct line, often referred to as the "endometrial stripe." The thickness of this stripe is carefully measured by your Gynecologist or sonographer. This measurement is crucial because changes in endometrial thickness can indicate various conditions, including hormonal imbalances or more serious concerns.
Interpreting Initial Findings: An Important Clue, Not a Final Verdict
It’s vital to understand that while a Transvaginal Ultrasound is incredibly informative, the finding of a thickened Endometrium is an indicator, not a definitive diagnosis of Endometrial Hyperplasia.
- What a Thickened Endometrium Suggests: A thicker-than-normal endometrial stripe can be a key clue that something is amiss, potentially signaling the presence of Endometrial Hyperplasia—a condition where the uterine lining grows excessively.
- Why It’s Not Definitive: However, various factors can cause endometrial thickening, including normal hormonal fluctuations during the menstrual cycle, hormone replacement therapy, or benign conditions like polyps or fibroids. Therefore, while a thickened Endometrium raises a red flag and warrants further investigation, it doesn’t automatically mean you have Endometrial Hyperplasia.
Why This Step is So Crucial
The Transvaginal Ultrasound stands as a crucial second step in your diagnostic journey for several compelling reasons:
- Non-Invasive Tool: It’s a non-surgical procedure, meaning it doesn’t involve incisions or a lengthy recovery, making it a safe and accessible first line of imaging.
- Informing Next Steps: The detailed information gathered from this ultrasound, especially regarding endometrial thickness, helps your Gynecologist make an informed decision. It allows them to assess the level of concern and determine if more conclusive and invasive testing, such as an Endometrial Biopsy, is truly necessary to arrive at a definitive diagnosis.
By providing a clear visual of your internal reproductive landscape, the Transvaginal Ultrasound helps to demystify your symptoms and pinpoint where further investigation might be needed, setting the stage for more definitive diagnostic steps.
After your transvaginal ultrasound has provided a detailed look at your uterine lining, the next crucial step often involves obtaining a physical sample for a definitive diagnosis.
Beyond the Image: The Definitive Answers an Endometrial Biopsy Provides
When concerns about the endometrium arise, seeing is often not enough – we need to understand what’s happening at a cellular level. This is where an endometrial biopsy becomes invaluable, offering the clearest picture of your uterine health.
What is an Endometrial Biopsy?
An Endometrial Biopsy is a medical procedure designed to obtain a small tissue sample directly from the endometrium, which is the lining of your uterus. Think of it as taking a tiny, targeted sample of cells to examine them closely. This procedure is considered the primary and most reliable method for gathering this vital tissue, especially when evaluating conditions like endometrial hyperplasia.
What to Expect During Your In-Office Biopsy
Understanding what happens during the biopsy can help ease any anxieties. The procedure is typically performed right in your doctor’s office, and while it might sound daunting, it’s a relatively quick process.
Here’s a general overview of what you can expect:
- Preparation: You’ll lie on an examination table, similar to a routine pelvic exam. Your doctor will use a speculum to gently open the vagina, allowing access to the cervix.
- Sampling: A very thin, flexible tube, sometimes called a pipelle, is carefully inserted through the cervix into the uterus.
- Collection: A gentle suction is applied through the tube to collect a small sliver of the uterine lining. This sample is incredibly tiny, about the size of a grain of rice.
- Sensation: Most women describe feeling some cramping during the procedure, similar to menstrual cramps. This sensation is usually brief, lasting only a minute or two while the sample is being collected. Some mild discomfort might linger afterward, but it typically subsides quickly.
Your doctor will guide you through each step, ensuring you’re as comfortable as possible. You might be advised to take over-the-counter pain medication, such as ibuprofen, about an hour before your appointment to help manage any potential cramping.
The Role of the Pathologist: Unveiling Cellular Secrets
Once the tissue sample is collected, your part in the procedure is complete. The delicate work then transitions to a specialized medical professional: the Pathologist.
Here’s how their expertise plays a crucial role:
- Laboratory Analysis: The tiny tissue sample is carefully preserved and sent to a pathology laboratory.
- Microscopic Examination: There, a pathologist, who is an expert in diagnosing diseases by examining tissues and bodily fluids, will meticulously prepare the sample. They then place it under a powerful microscope.
- Detailed Assessment: Under the microscope, the pathologist carefully examines the cells for any abnormalities. They look for changes in cell size, shape, organization, and growth patterns that might indicate endometrial hyperplasia or other conditions.
Why This Test Is Definitive
The endometrial biopsy stands as the "gold standard" for diagnosis for a very important reason: it offers definitive answers that other tests cannot.
- Confirmation of Endometrial Hyperplasia: While imaging like ultrasound can suggest the presence of hyperplasia, only a biopsy can definitively confirm it by examining the actual tissue.
- Detection of Atypical Cells: Most importantly, the pathologist can identify if atypical cells are present within the endometrial sample. Atypical cells are abnormal cells that have a higher potential to progress to cancer. This distinction is critical because the presence or absence of atypical cells directly influences treatment recommendations.
In essence, the endometrial biopsy moves beyond imaging to provide a clear, microscopic view of your uterine lining, delivering the precise information needed to understand your condition and plan the most appropriate care.
With the detailed insights from your endometrial biopsy, we can then consider further advanced diagnostic steps, such as a hysteroscopy and D&C, if needed.
While the endometrial biopsy offers a crucial first look, sometimes the path to clarity requires a more detailed exploration.
When the First Glimpse Isn’t Enough: Unveiling Deeper Insights with Hysteroscopy and D&C
Understanding your health journey means sometimes taking a closer look, especially when initial answers are unclear. When a standard endometrial biopsy doesn’t provide all the necessary information, or if there’s a strong suspicion of certain conditions, your doctor may recommend more advanced diagnostic procedures like a hysteroscopy and a Dilation and Curettage (D&C). These steps allow for a more thorough investigation, ensuring you get the most accurate picture of your uterine health.
Why Sometimes We Need to Look Closer
An endometrial biopsy is an excellent screening tool, but it involves taking a small, "blind" sample from the uterine lining. This means it might miss certain areas or not gather enough tissue to make a definitive diagnosis. There are specific scenarios where your doctor might recommend further testing:
- Inconclusive Biopsy Results: Sometimes, the tissue sample from a biopsy might be insufficient for analysis, or the results are unclear, leaving your doctor and you with unanswered questions.
- Persistent Symptoms: If you continue to experience abnormal bleeding or other concerning symptoms even after a "normal" biopsy, it suggests there might be something deeper that wasn’t captured in the initial sample.
- High Suspicion: Based on other factors like ultrasound findings (e.g., thickened uterine lining, polyps), your medical history, or specific risk factors for uterine conditions, your doctor might have a high suspicion of atypical hyperplasia (a precancerous condition) or endometrial cancer, warranting a more comprehensive evaluation.
- Specific Abnormalities: If an ultrasound or prior biopsy indicated the presence of polyps, fibroids, or other growths, a hysteroscopy can visually confirm and assess these.
A Guided Tour: Understanding Hysteroscopy
Imagine being able to look directly inside your uterus – that’s essentially what a hysteroscopy allows us to do. It’s a procedure where a very thin, lighted tube with a camera at its tip, called a hysteroscope, is gently inserted through your vagina and cervix into your uterus.
During a hysteroscopy, your doctor can:
- Visually Inspect: Carefully examine the entire inner lining of the uterus (the endometrium) for any abnormalities that might have been missed by a blind biopsy.
- Identify Issues: Pinpoint specific areas of concern, such as polyps (non-cancerous growths), fibroids (benign muscle tumors), scar tissue, or areas that look suspicious for precancerous changes or cancer.
- Target Biopsies: If an abnormal area is identified, the doctor can perform a targeted biopsy, taking a precise tissue sample directly from that specific spot for laboratory analysis. This offers much more accuracy than a blind biopsy.
Collecting a Wider Sample: What is a D&C?
A Dilation and Curettage (D&C) is another important procedure often performed alongside a hysteroscopy, or sometimes on its own. It’s a minor surgical procedure designed to remove a larger, more comprehensive sample of the endometrial lining for analysis.
During a D&C:
- Dilation: The cervix (the opening to the uterus) is gently dilated, or widened, to allow instruments to pass through.
- Curettage: A small, spoon-shaped instrument called a curette, or sometimes a suction device, is then used to carefully scrape or suction the lining of the uterus. This collects a more extensive tissue sample compared to a standard biopsy.
Often, a D&C is performed under visual guidance with a hysteroscopy. This "see and scrape" approach allows the doctor to visually identify problem areas and then ensure a thorough collection of tissue from those and surrounding regions, maximizing the chances of an accurate diagnosis.
Working Together for Clarity: Hysteroscopy and D&C
These advanced diagnostic tools provide a much more thorough evaluation than a standalone biopsy. Hysteroscopy offers the invaluable benefit of direct visualization, allowing your doctor to "see" the problem. A D&C, especially when guided by hysteroscopy, ensures that a sufficient and representative tissue sample is collected from the entire uterine lining, or from specific suspicious areas.
Together, they significantly increase the accuracy of diagnosis, particularly when there’s a high suspicion of atypical hyperplasia (a precancerous condition) or endometrial cancer. They help confirm or rule out these conditions with greater certainty, guiding the next steps in your care.
To help clarify the unique contributions of each procedure, here’s a comparison:
Comparing Hysteroscopy and Dilation and Curettage (D&C)
| Feature | Hysteroscopy | Dilation and Curettage (D&C) |
|---|---|---|
| Purpose | Visually inspect the uterine cavity, identify abnormalities, perform targeted biopsies. | Obtain a comprehensive tissue sample of the uterine lining, remove small growths. |
| Procedure Type | Diagnostic; involves a thin, lighted camera (hysteroscope) inserted into the uterus. | Diagnostic/Therapeutic; involves dilating the cervix and gently scraping or suctioning the uterine lining. |
| What it Reveals | Direct visualization of polyps, fibroids, scar tissue, and suspicious lesions; precise location for biopsy. | Presence and extent of abnormal cells (e.g., atypical hyperplasia, endometrial cancer); can remove small polyps or tissue remnants. |
| Often Performed | Can be standalone, or immediately followed by a D&C. | Often performed in conjunction with a hysteroscopy for guided tissue collection. |
Once these advanced procedures are complete, the collected tissue samples embark on their journey to the pathology lab.
After the diagnostic steps of hysteroscopy and D&C, the next crucial phase involves understanding what those procedures revealed about your health.
Decoding the Diagnosis: Your Pathology Report, Demystified
Following a biopsy or D&C, the tissue samples collected are sent to a specialized laboratory, marking a pivotal moment in your diagnostic journey. This is where the Pathology Report comes into play – it’s the definitive document that provides the expert microscopic analysis of your cells, offering the precise diagnosis from a Pathologist. Think of it as the final piece of the puzzle, translating the visible findings into a clear medical explanation of your condition.
Unpacking Your Pathology Report: The Language of Cells
Your pathology report will describe the characteristics of the endometrial cells found in your sample. The primary concern is often the presence and type of endometrial hyperplasia, a condition where the lining of the uterus (endometrium) becomes abnormally thick due to an overgrowth of cells. Understanding the specific classification is vital, as it directly impacts your risk and treatment strategy.
Hyperplasia Without Atypia: A Less Concerning Picture
When your report indicates Hyperplasia without Atypia, it means that while there’s an increased number of endometrial cells, their individual structure and appearance are still relatively normal. They might be numerous, but they don’t show the worrisome changes that suggest a progression towards cancer.
- Key Characteristics: Increased number of cells, but cells retain their normal shape and organization.
- Risk Profile: This is considered the less concerning form of hyperplasia. It has a very low risk of progressing to Endometrial Cancer, often less than 5% over 20 years.
- Management: Often managed with hormonal therapy (progestins) or close monitoring.
The Critical Distinction: Atypical Hyperplasia
Conversely, a diagnosis of Atypical Hyperplasia carries a significantly different weight. This is where the pathologist identifies not just an increase in cell number, but also structural abnormalities within the cells themselves. These "atypical" changes are considered precancerous, meaning they have a higher potential to evolve into Endometrial Cancer.
- Key Characteristics: Increased number of cells, plus the individual cells show abnormal shapes, sizes, and organization (e.g., larger nuclei, prominent nucleoli, irregular membranes).
- Risk Profile: This is the more serious form of hyperplasia, directly categorized as a precancerous condition. The risk of progressing to Endometrial Cancer is substantially higher, ranging from 10% to 50% or more, depending on whether it’s classified as "simple" or "complex" atypical hyperplasia. In fact, a small percentage of cases diagnosed as atypical hyperplasia may even have concurrent undiagnosed cancer at the time of biopsy.
- Management: Due to the significantly higher risk, treatment often involves more aggressive approaches, potentially including a hysterectomy for definitive removal, especially in postmenopausal women or those who have completed childbearing.
Understanding Your Specific Results
To help clarify the different types of endometrial hyperplasia and their implications, the table below provides a summary of common classifications, their features, and the associated risks.
| Type of Endometrial Hyperplasia | Key Characteristics | Risk of Progressing to Endometrial Cancer (Approximate) |
|---|---|---|
| Simple Hyperplasia | Glands are increased in number and size, but remain well-organized and cells are normal. | <1% |
| Complex Hyperplasia | Glands are crowded and show irregular shapes, but cells are still normal. | 3-5% |
| Simple Atypical Hyperplasia | Glands are increased, may be crowded, and cells show structural abnormalities (atypia). | 8-10% |
| Complex Atypical Hyperplasia | Glands are crowded, irregular, and cells show significant structural abnormalities (atypia). | 20-50% (and up to 40% may have concurrent cancer) |
It’s paramount to remember that this report is intensely personal and holds profound implications for your health. The most critical next step is to sit down with your Gynecologist and discuss the report thoroughly. They will explain the specific type of hyperplasia you have, what these findings mean for your individual situation, and outline the potential paths forward for your treatment plan. This detailed conversation will empower you to make informed decisions about your care.
Once you have a clear understanding of your diagnosis, the focus shifts to crafting a personalized strategy for your health and well-being.
Once you’ve meticulously deciphered your pathology report and grasped its findings, the natural question arises: "What happens next?"
From Report to Roadmap: Crafting Your Personalized Health Strategy
Receiving a diagnosis can feel like a significant moment, marking the end of uncertainty but the beginning of a new phase. This phase is not about facing challenges alone, but about forging a strong partnership with your healthcare team to design your path forward. It’s about translating the detailed findings of your pathology report into a proactive, personalized health strategy.
Reflecting on Your Journey: From Symptoms to Diagnosis
Your journey to this point has been a testament to your proactive approach to health. It typically involves a series of crucial steps, each building upon the last to provide a comprehensive understanding of your condition:
- Initial Symptoms and Concerns: It all begins with recognizing changes in your body, such as unusual bleeding patterns or discomfort, prompting you to seek medical advice.
- Doctor Consultation and Assessment: Your first visit to a healthcare provider involves discussing your symptoms, medical history, and a physical examination.
- Diagnostic Testing: This often includes various tests like ultrasounds or blood work to gather more information and narrow down possibilities.
- The Biopsy: A pivotal step where a small tissue sample (e.g., an endometrial biopsy) is carefully collected for microscopic examination.
- The Pathology Report: The culmination of this process, where a specialized doctor (pathologist) analyzes the tissue and provides a definitive diagnosis, detailing the specific characteristics of any abnormal cells.
Understanding these steps helps reinforce that your diagnosis is the product of a thorough and careful investigative process, not an arbitrary label.
Navigating Treatment Options: A Tailored Approach
The specific recommendations for your next steps depend entirely on the precise nature of your diagnosis. Each condition, even within a similar category, warrants a unique approach:
Hyperplasia Without Atypia
If your pathology report indicates hyperplasia without atypia, meaning there’s an overgrowth of cells but no abnormal or "atypical" features that suggest a higher risk of cancer, your treatment plan will often focus on managing the cellular overgrowth and preventing progression. A common and effective treatment for this is:
- Progestin Therapy: This involves using synthetic forms of the hormone progesterone (progestin) to counteract the effects of estrogen, which often stimulates endometrial growth. Progestin can help to thin the uterine lining, reducing the hyperplasia. This can be administered in various forms, such as oral pills, an intrauterine device (IUD) that releases progestin directly into the uterus, or injections. Your doctor will discuss the most suitable option for you based on your individual circumstances and preferences.
Addressing Atypical Hyperplasia
A diagnosis of atypical hyperplasia carries a more significant implication and often necessitates a more assertive management strategy. This is because atypical hyperplasia indicates not just an overgrowth of cells, but also the presence of abnormal, "atypical" features within those cells. These atypical cells have a considerably higher risk of either:
- Co-existing Endometrial Cancer: Meaning cancer may already be present in other areas of the uterus, even if not fully captured in the biopsy.
- Future Endometrial Cancer Development: Atypical hyperplasia is considered a precursor to endometrial cancer, meaning there’s a substantially increased chance of it progressing to cancer over time if not adequately treated.
Due to these elevated risks, your doctor will discuss more definitive treatment options, which might include surgery (such as a hysterectomy), close surveillance, or higher-dose progestin therapy, depending on factors like your age, desire for future fertility, and overall health.
Your Path Forward: Empowerment Through Partnership
A diagnosis is never an endpoint; rather, it is the crucial first step toward developing a proactive health plan tailored specifically for you. It provides clarity and direction, empowering you to make informed decisions about your health. Remember, you are not alone in this. Your healthcare team—your doctor, nurses, and other specialists—are your dedicated partners. They are there to explain your diagnosis in detail, outline all available treatment options, answer your questions, and support you every step of the way.
Embrace open communication with your healthcare provider. Don’t hesitate to ask questions, share your concerns, and express your preferences. Together, you will navigate this journey, finding the best path forward that aligns with your health goals and personal values, ensuring you have the support and information needed for your continued well-being.
Frequently Asked Questions About Endometrial Hyperplasia Diagnosis: What Are the 5 Key Steps?
What is the first step in endometrial hyperplasia diagnosis?
The initial step often involves a transvaginal ultrasound to assess the thickness of the endometrium. An abnormally thick lining may indicate the need for further investigation regarding endometrial hyperplasia diagnosis.
What kind of biopsy is typically performed for endometrial hyperplasia diagnosis?
An endometrial biopsy is the standard procedure, where a small tissue sample is taken from the uterine lining. This sample is then examined under a microscope to determine if endometrial hyperplasia is present.
What happens after a diagnosis of endometrial hyperplasia?
Following an endometrial hyperplasia diagnosis, the next step is determining the type and grade. This is crucial because it informs the best course of treatment, which can range from hormone therapy to hysterectomy.
How important is follow-up after treatment for endometrial hyperplasia?
Regular follow-up is critical after treatment for endometrial hyperplasia. This helps monitor for any recurrence or progression, and ensures the effectiveness of the chosen treatment strategy.
Navigating a potential diagnosis of Endometrial Hyperplasia can feel like a complex journey, but by understanding the 5 key steps—from recognizing symptoms and your initial Gynecologist consultation, through advanced diagnostics like Transvaginal Ultrasound and the definitive Endometrial Biopsy, and finally to decoding your Pathology Report—you are now empowered with crucial knowledge.
Remember, a diagnosis isn’t an endpoint; it’s the critical first step toward a proactive health plan tailored specifically for you. Your path forward will depend entirely on your specific diagnosis. For hyperplasia without atypia, your doctor might discuss options like Progestin Therapy. However, if Atypical Hyperplasia is identified, more assertive management is often recommended due to its higher risk of progression to Endometrial Cancer.
Above all, maintain open communication with your healthcare team. Ask questions, share your concerns, and work collaboratively to determine the best treatment and monitoring strategy for your unique situation. You are not alone on this journey, and being well-informed is your strongest ally.