Understanding changes in sexual function is a key aspect of post-operative care following a hysterectomy. Many women wonder about self-stimulation after hysterectomy, and it’s completely valid to question what’s normal. The role of pelvic floor therapy in recovery is significant, and understanding how it supports overall well-being is crucial. Considering these factors helps in maintaining a healthy and fulfilling life while addressing any concerns about self-stimulation after hysterectomy.
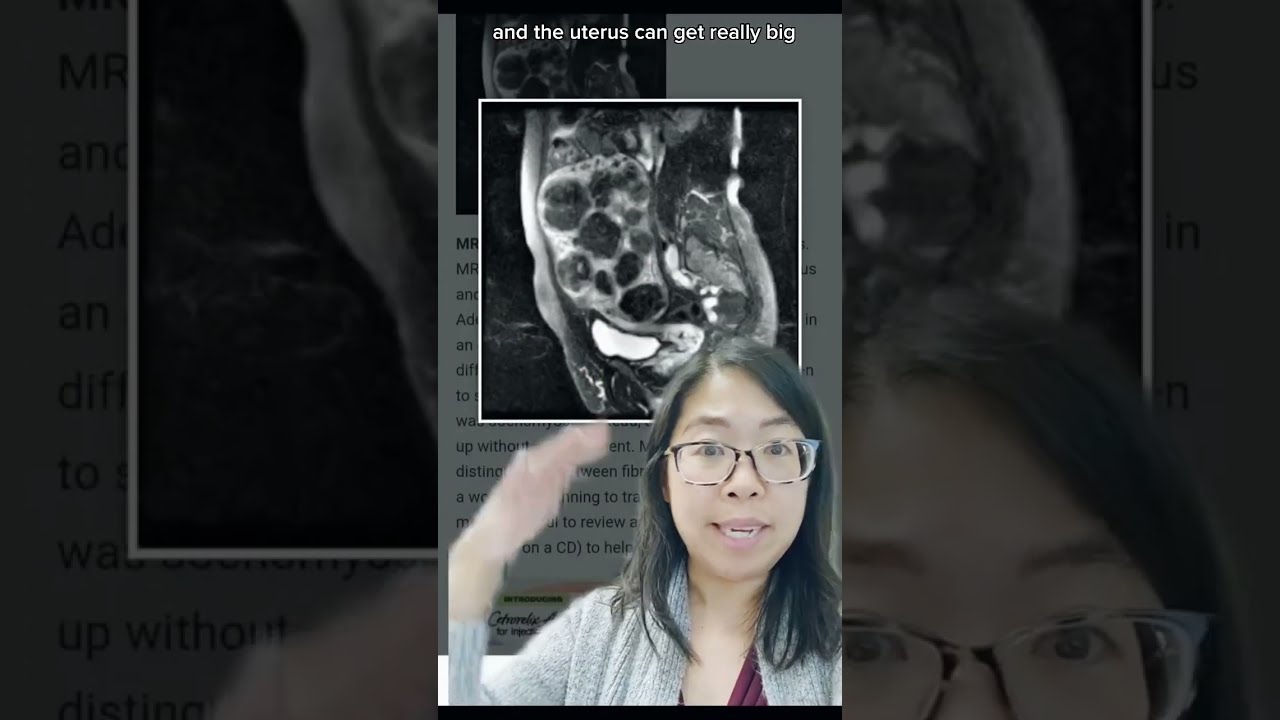
Image taken from the YouTube channel Karen Tang, MD , from the video titled What happens to the *space* where the uterus was after a HYSTERECTOMY? Gynecologist Explains! #short .
Navigating life after a hysterectomy involves many adjustments, both physical and emotional. One area that often raises questions, yet remains shrouded in silence, is sexual function, specifically self-stimulation.
It’s completely understandable to have concerns and seek clarity on this topic. Many women find themselves wondering: Is it normal? Is it safe? Will it feel the same?
Acknowledging the Sensitivity and Common Questions
Let’s be frank: talking about self-stimulation, or masturbation, even in the context of post-operative recovery, can feel vulnerable. There’s a lingering societal discomfort around female sexuality that makes open discussion challenging.
It’s important to acknowledge this sensitivity upfront. The questions you have about sexual function after a hysterectomy are valid and deserve straightforward answers.
Many women experience concerns related to:
- Changes in sensation.
- Pain or discomfort.
- Decreased libido.
- Body image issues.
- The impact on their relationships.
Purpose: Providing Clear and Factual Information
This article aims to provide clear, factual information about self-stimulation after a hysterectomy. We’ll address common concerns, explore the physiological and emotional factors at play, and offer reassurance that prioritizing your sexual well-being is a normal and healthy part of post-operative life.
This is about empowering you with knowledge.
Reassurance Amidst Concerns and Anxieties
It’s natural to feel anxious or uncertain about how a hysterectomy might affect your sexual life. Know that you are not alone in these feelings. Many women experience similar concerns.
The goal here is to offer reassurance and dispel any myths or misconceptions.
By understanding the changes your body is undergoing and how to adapt, you can continue to enjoy a fulfilling and pleasurable sexual life after a hysterectomy. We’ll guide you through these considerations, ensuring you feel informed and confident in your journey toward sexual well-being.
Let’s move on to understanding the procedure itself and its potential effects on your body and emotions.
Understanding Hysterectomy: Types and Impacts
A hysterectomy is a surgical procedure involving the removal of the uterus. It’s a significant decision with lasting implications, so understanding the different types and their potential effects is crucial.
Defining Hysterectomy: A Detailed Look
At its core, a hysterectomy is the surgical removal of the uterus. This means that after the procedure, a woman will no longer be able to get pregnant.
The procedure is typically performed to address various health conditions, including:
- Fibroids
- Endometriosis
- Uterine prolapse
- Certain cancers
Types of Hysterectomy: Choosing the Right Approach
Not all hysterectomies are the same. The specific type of hysterectomy performed depends on the individual’s medical condition and overall health. Here’s a breakdown of the common types:
Partial Hysterectomy
In a partial hysterectomy, also known as a supracervical hysterectomy, only the upper part of the uterus is removed. The cervix is left intact.
Total Hysterectomy
A total hysterectomy involves the removal of the entire uterus and the cervix. This is the most common type of hysterectomy.
Radical Hysterectomy
A radical hysterectomy is the most extensive type of hysterectomy. It involves the removal of the uterus, cervix, the upper part of the vagina, and surrounding tissues, including lymph nodes.
This type is typically performed in cases of cancer.
Oophorectomy and Salpingectomy
It’s also important to note that a hysterectomy may be performed with other procedures, such as an oophorectomy (removal of the ovaries) or a salpingectomy (removal of the fallopian tubes).
These procedures can significantly impact hormone levels and overall health.
Physical and Emotional Effects: Navigating the Changes
A hysterectomy is a major surgical procedure, and it can have both physical and emotional effects. It’s important to be prepared for these changes and to seek support when needed.
Physical Impacts
Physically, a hysterectomy can lead to:
- Pain and discomfort
- Fatigue
- Changes in bowel and bladder function
If the ovaries are removed, it can also lead to menopausal symptoms, such as hot flashes, vaginal dryness, and mood swings.
Emotional Impacts
Emotionally, a hysterectomy can be a complex experience. Some women may feel relieved to be free of the symptoms that led to the surgery. Others may experience feelings of loss, grief, or anxiety.
Changes in body image and concerns about sexual function can also contribute to emotional distress.
It’s crucial to acknowledge these feelings and seek support from loved ones, therapists, or support groups.
The Recovery Process: Prioritizing Your Well-being
The recovery process after a hysterectomy is crucial for healing and regaining your quality of life.
Rest is essential in the initial weeks following surgery. Follow your doctor’s instructions carefully regarding activity restrictions, pain management, and wound care.
It’s also vital to prioritize your emotional well-being during this time. Engage in activities that bring you joy, practice self-care, and seek support from others.
Remember that recovery is a process, and it’s okay to ask for help along the way.
Of course, here is the outline you requested:
Is Self-Stimulation Normal After Hysterectomy? The Straight Answer
With a clearer understanding of what a hysterectomy entails and its various forms, the natural next question that arises is: what about intimacy and sexual function after the procedure? This is a common and valid concern.
Let’s address the core question head-on.
Yes, self-stimulation after a hysterectomy is perfectly normal and healthy.
It’s a natural part of human sexuality, and a hysterectomy doesn’t inherently change that. The ability to experience pleasure and orgasm typically remains intact.
Orgasm After Hysterectomy: What to Expect
The uterus itself isn’t directly responsible for orgasm.
Instead, the clitoris, vagina, and other erogenous zones are the primary players in sexual arousal and pleasure.
Because a hysterectomy doesn’t necessarily impact these areas, the capacity to experience orgasm remains.
Many women report continuing to enjoy satisfying sexual experiences, including self-stimulation, after their recovery.
Factors Influencing Sexual Function Post-Hysterectomy
While the potential for sexual function remains after a hysterectomy, several factors can influence a woman’s experience:
- Hormonal Changes: Depending on whether the ovaries were removed during the hysterectomy (oophorectomy), there may be hormonal shifts that impact libido.
- Nerve Damage: Although rare, nerve damage during surgery can affect sensation and arousal.
- Emotional Factors: Body image concerns, anxiety, or depression related to the surgery can play a significant role in sexual desire and function.
- Relationship Dynamics: Changes in sexual function can also be related to relationship dynamics with a partner.
- Pelvic Floor Health: The pelvic floor muscles play a role in sexual function, and their strength and tone can affect sensation and orgasm.
It’s also important to allow adequate time for physical healing.
Trying to resume sexual activity too soon after surgery can cause discomfort or pain, which will lead to a negative association.
Patience and gentle exploration are key.
The ability to experience sexual pleasure after a hysterectomy is closely linked to several physiological factors. Understanding these factors can help women navigate their post-operative sexual health with greater awareness and confidence. Let’s explore the key components: the vagina, clitoris, pelvic floor, and the critical roles hormones play in libido and sexual response.
Physiological Factors: Vagina, Clitoris, Hormones, and Libido
The Vagina and Clitoris: Centers of Pleasure
The vagina and clitoris are primary players in female sexual arousal and orgasm.
The vagina, with its network of nerve endings, responds to stimulation through touch and pressure. During self-stimulation, whether through direct contact or the use of sexual aids, these nerve endings send signals to the brain, initiating the arousal process.
The clitoris, often described as the female equivalent of the penis, is packed with thousands of nerve endings.
It is the most sensitive erogenous zone in the female body.
Direct or indirect stimulation of the clitoris leads to increased blood flow, swelling, and heightened sensitivity, ultimately contributing to orgasm.
A hysterectomy, by itself, does not directly impair the function of either the vagina or clitoris unless there’s unforeseen nerve damage, which is rare. Therefore, the potential for experiencing pleasure through these organs usually remains intact.
The Role of the Pelvic Floor
Often overlooked, the pelvic floor muscles play a crucial role in sexual function.
These muscles support the pelvic organs, including the vagina and uterus (before a hysterectomy), and contribute to sexual sensation and orgasm.
During arousal, the pelvic floor muscles contract and relax, enhancing blood flow to the pelvic region and increasing sensitivity.
At the point of orgasm, these contractions become more intense and rhythmic, contributing to the pleasurable sensations experienced.
A hysterectomy can indirectly affect the pelvic floor muscles.
The removal of the uterus can sometimes lead to weakening or changes in these muscles.
Pelvic floor exercises, such as Kegels, can help strengthen these muscles, improving sexual function and overall pelvic health post-surgery.
Hormonal Impact on Libido and Sexual Response
Hormones, particularly estrogen and testosterone, are powerful drivers of libido (sex drive) and sexual response in women.
Estrogen plays a vital role in vaginal lubrication, elasticity, and blood flow to the pelvic region. It also influences mood and overall sexual desire.
Testosterone, although often associated with men, is also present in women and contributes significantly to libido, sexual arousal, and orgasm.
If the ovaries are removed during a hysterectomy (oophorectomy), there can be a significant drop in estrogen and testosterone levels.
This hormonal shift can lead to a variety of symptoms, including decreased libido, vaginal dryness, and difficulty achieving orgasm.
Even when the ovaries are conserved, they may experience a temporary dip in hormone production post-surgery due to altered blood supply.
Addressing Decreased Libido
Decreased libido after a hysterectomy can be a challenging, but not insurmountable, issue. Here are some management strategies:
- Hormone Therapy (HT): If the ovaries were removed, hormone therapy can help replenish estrogen levels, alleviating symptoms such as vaginal dryness and decreased libido. Discuss the risks and benefits with your healthcare provider to determine if HT is right for you.
- Vaginal Estrogen: For localized vaginal dryness, topical estrogen creams or suppositories can be applied directly to the vagina to improve lubrication and elasticity.
- Testosterone Therapy: In some cases, testosterone therapy may be considered to boost libido, especially if testosterone levels are low. However, it’s crucial to discuss the potential side effects with a medical professional.
- Lifestyle Modifications: Adopting a healthy lifestyle can positively impact libido. This includes regular exercise, a balanced diet, adequate sleep, and stress management techniques.
- Open Communication: Talking openly with your partner about your sexual needs and concerns can strengthen intimacy and improve sexual satisfaction.
- Counseling or Sex Therapy: A therapist can provide guidance and support in addressing emotional or psychological factors that may be contributing to decreased libido. They can also offer techniques to enhance sexual arousal and pleasure.
- Explore Alternative Therapies: Some women find relief through alternative therapies such as acupuncture, yoga, or herbal remedies. It’s essential to discuss these options with your doctor to ensure they are safe and appropriate for you.
By understanding the physiological factors that influence self-stimulation and sexual function after a hysterectomy, women can take proactive steps to maintain their sexual health and well-being. Remember, seeking guidance from healthcare professionals is key to addressing any concerns and finding solutions that work best for your individual needs.
The pelvic floor muscles, working in concert with the vagina and clitoris, intensify the sensations experienced during self-stimulation. Strengthening these muscles through exercises like Kegels can enhance sexual responsiveness and contribute to more satisfying orgasms. Now, let’s turn our attention to the emotional and psychological landscape that influences a woman’s experience with self-stimulation after a hysterectomy.
Emotional and Psychological Considerations: Body Image and Intimacy
A hysterectomy is more than just a surgical procedure; it’s a life event that can profoundly impact a woman’s sense of self. The emotional and psychological repercussions of a hysterectomy often extend to one’s body image and intimate relationships, significantly influencing the ability to engage in and enjoy self-stimulation. It’s crucial to acknowledge these non-physical dimensions of sexual health and well-being.
The Interplay of Body Image and Self-Esteem
Body image, the perception and feelings one has about their physical self, can be significantly affected after a hysterectomy.
Some women may struggle with feelings of loss, incompleteness, or a diminished sense of femininity following the procedure.
These feelings can stem from the removal of the uterus, an organ closely associated with reproduction and womanhood.
Negative body image can lead to decreased self-esteem, making it challenging to feel comfortable and confident in one’s own skin.
This, in turn, can negatively impact sexual desire and the willingness to engage in self-stimulation.
It’s important to understand that these feelings are valid and common.
Reclaiming Your Body: Self-Acceptance and Empowerment
Overcoming negative body image requires a conscious effort toward self-acceptance and empowerment. This may involve:
- Self-compassion: Treating yourself with the same kindness and understanding you would offer a friend.
- Focusing on strengths: Identifying and appreciating your physical and emotional attributes.
- Challenging negative thoughts: Actively refuting negative self-talk and replacing it with positive affirmations.
- Engaging in self-care: Prioritizing activities that promote physical and emotional well-being, such as exercise, healthy eating, and relaxation techniques.
Intimacy and Communication in Relationships
A hysterectomy can also impact intimate relationships, particularly if there are unresolved feelings or communication barriers.
Open and honest communication with your partner is essential for navigating these challenges.
Discussing your feelings, needs, and concerns can foster understanding and strengthen the emotional bond between you and your partner.
- Expressing your needs: Clearly communicate your desires and preferences regarding sexual activity.
- Listening actively: Pay attention to your partner’s feelings and concerns without judgment.
- Seeking professional support: If communication is difficult, consider seeking guidance from a therapist or counselor.
Rekindling Intimacy: Exploring New Pathways to Connection
Intimacy encompasses more than just sexual activity; it includes emotional closeness, shared experiences, and mutual support.
After a hysterectomy, couples may need to explore new ways to connect and maintain intimacy.
This could involve:
- Prioritizing quality time together: Engaging in activities that foster closeness and connection, such as cuddling, talking, or pursuing shared hobbies.
- Exploring non-sexual intimacy: Focusing on sensual touch, massage, or other forms of physical affection that do not necessarily lead to sexual activity.
- Experimenting with new forms of sexual expression: Trying different positions, techniques, or incorporating sex toys to enhance pleasure and satisfaction.
The Power of Self-Exploration
Self-stimulation can be a powerful tool for rediscovering your body and reclaiming your sexuality after a hysterectomy.
It allows you to explore your erogenous zones, identify what feels good, and regain confidence in your ability to experience pleasure.
Remember, self-stimulation is not just about physical gratification; it’s also about self-discovery, self-acceptance, and self-love. It can be a positive and empowering experience that enhances your overall well-being.
Emotional and psychological well-being play a vital role in a woman’s experience with self-stimulation and overall sexual health following a hysterectomy. By fostering a positive body image and maintaining open communication, women can navigate these changes with greater ease and confidence.
Seeking Professional Guidance: When to Consult a Specialist
While self-exploration and open communication are invaluable, there are times when seeking professional guidance becomes essential. It’s important to recognize that navigating the changes after a hysterectomy can be complex, and specialized support can make a significant difference in your journey toward sexual well-being.
The Value of Expert Consultation
Consulting with healthcare providers, such as gynecologists and sex therapists, provides access to personalized advice and support tailored to your specific needs and circumstances.
These professionals possess the expertise to address both the physical and emotional aspects of sexual health, offering insights and strategies that can empower you to regain control and enhance your sexual experiences.
A gynecologist can assess your physical health, rule out any underlying medical conditions, and discuss potential treatments or interventions.
A sex therapist, on the other hand, specializes in addressing the psychological and emotional factors that can influence sexual function and satisfaction.
Recognizing When to Seek Help
Knowing when to seek professional help is crucial. While some challenges may resolve on their own with time and self-care, persistent or worsening issues warrant expert attention.
Here are some specific scenarios where consulting a healthcare provider is highly recommended:
- Persistent Pain During Self-Stimulation or Intercourse: Pain is never normal and should always be investigated. A gynecologist can identify the cause of the pain and recommend appropriate treatment options.
- Significantly Decreased Sex Drive (Libido): While some fluctuation in libido is normal, a significant and persistent decrease can be a sign of hormonal imbalances or other underlying issues. A healthcare provider can assess your hormone levels and explore potential solutions.
- Difficulty Achieving Orgasm: If you are consistently experiencing difficulty achieving orgasm despite adequate stimulation, it may be beneficial to consult with a sex therapist. They can help identify any psychological or emotional factors contributing to this issue and provide strategies for enhancing your orgasmic response.
- Emotional Distress or Anxiety Related to Sexual Function: Feelings of anxiety, depression, or inadequacy related to your sexual function should not be ignored. A therapist can provide a safe and supportive space to explore these emotions and develop coping mechanisms.
- Relationship Issues Related to Sexual Intimacy: If changes in your sexual function are impacting your relationship, couples therapy can be a valuable resource. A therapist can help you and your partner communicate openly, address any underlying issues, and find ways to reconnect intimately.
- Uncertainty or Confusion About Your Sexual Health: If you have questions or concerns about your sexual health that you are unable to address on your own, consulting with a healthcare provider can provide clarity and reassurance.
Empowering Yourself Through Professional Support
Seeking professional guidance is not a sign of weakness but rather an act of self-care and empowerment.
It demonstrates a commitment to prioritizing your sexual health and well-being and taking proactive steps to address any challenges you may be facing.
By partnering with healthcare professionals, you can gain the knowledge, support, and tools you need to navigate the changes after a hysterectomy and reclaim your sexual confidence.
FAQs: Self-Stimulation After Hysterectomy
Got questions about self-stimulation after a hysterectomy? Here are some answers to common concerns.
Is it normal to experience changes in sexual desire after a hysterectomy?
Yes, it’s common. A hysterectomy can impact hormone levels, potentially affecting sexual desire. However, it’s different for everyone; some women experience increased desire, while others see a decrease. Factors such as age and whether the ovaries were removed also play a role.
Is self-stimulation after hysterectomy safe?
Generally, yes. Unless your doctor has given specific instructions to avoid sexual activity, self-stimulation after hysterectomy is usually safe once you’ve recovered from surgery. Follow your doctor’s post-operative guidelines regarding physical activity.
Can self-stimulation after hysterectomy help with recovery?
While it won’t directly heal surgical wounds, some women find that self-stimulation after hysterectomy can help them reconnect with their bodies and improve mood through endorphin release. This can contribute to overall well-being during recovery.
What if I experience pain or discomfort during self-stimulation after hysterectomy?
If you experience pain or discomfort, stop immediately. It’s possible that you’re still healing. Discuss your concerns with your doctor. They can assess your recovery and offer tailored advice.
So, that’s the lowdown on self-stimulation after hysterectomy! Hopefully, you’ve got a better understanding now. Always listen to your body, and don’t hesitate to chat with your doctor if you have any more questions. Take care!